In a fresh look at healthcare quality in the United States from the eyes of the nation’s healthcare quality professionals, is a view of healthcare organizations’ training and development of their employees’ capabilities in delivering quality healthcare.
In its inaugural survey of healthcare quality, NAHQ asked healthcare quality professionals which employees in their organization receive training and education on quality.
Only 33 percent of respondents said all staff receive training and education on quality within their healthcare organization.
The survey also asked respondents the one thing they would do to improve quality at their organization. Nearly half, or 47 percent, said their healthcare organizations need to align all healthcare professionals.
Respondents to the survey are healthcare quality professionals in the United States, the majority of whom work in hospitals and for whom quality improvement is their day-to-day work. They know healthcare quality improvement better than any other healthcare professionals through their training, development and experience in healthcare organizations.
Separately, more and more healthcare disciplines and specialties are increasing quality and safety training for their own professionals. NAHQ praises these efforts, says Executive Director and CEO, Stephanie Mercado, but points out that discipline or specialty specific training can unintentionally create vertical silos that don’t optimize team-based, patient care delivery.
Healthcare silos that affect quality can be overcome.
Trained and certified healthcare quality professionals are the primary building block in breaking down the barriers that disrupt quality because they both harmonize the workforces contributing to quality and provide the essential link from front-line care to corporate business objectives. However, to advance healthcare quality fully, in a way that improves both patient and financial outcomes consistent with the goals of healthcare value, Mercado says the entire workforce, regardless of specialty, discipline or role, has to speak the same language of quality, which will only come when everyone is trained on industry-standard quality competencies.
The NAHQ survey is the most recent of the association’s efforts to raise awareness of improvements that will advance Quality Driven Healthcare. NAHQ hosted a fourth quarter 2018 roundtable of healthcare executives that resulted in a Call-to-Action for quality workforce integration. As the convener of the conversation on the critical importance of workforce alignment on quality, NAHQ will gather healthcare executives at its National Healthcare Quality Summit on May 2-3, 2019, in Chicago, to discuss the value of a healthcare workforce trained in quality competencies, and will provide specific examples of the positive results achieved by healthcare organizations who have made this commitment.
Cathy Duquette, PhD RN NEA-BC CPHQ FNAHQ, Executive Vice President, Nursing Affairs and Nidia Williams, PhD MBB CPHQ FNAHQ, Vice President, Operational Excellence of Lifespan will discuss their health system’s experience of reorganization to focus on quality competencies defined by NAHQ. They will share how Lifespan made the transition that resulted in $12M saved over four years’ time and vastly improved patient safety.
Paul Stefanacci, MD FACS MBA, Vice President, Quality and Chief Medical Officer and Ted Donnelly, MHA BSN, Director, Quality, Acute Care Division of Universal Health Services (UHS), will discuss their health system’s corporate commitment to a quality competency-based workforce. UHS has found that quality improves and remains sustainable when staff shares the same vocabulary and competencies for quality through consistent, structured education and training. UHS has deployed NAHQ’s resources that include multi-stakeholder training and development on quality competencies to close the gaps and eliminate variability between different approaches in the workforce.
Brad Neet, MBA RN BSN, Chief Executive Officer and Nikole DeVries, MSN RN CPHQ, Director, Performance Improvement and Patient Engagement of Southwest Healthcare System, a subsidiary of UHS currently comprised of two hospitals, will talk about how quality competencies have been employed at their institution.
Executives interested in NAHQ’s Healthcare Quality Summit can request an invitation to this event by contacting Tpyle@nahq.org. More information is also available at NAHQSummit.org.
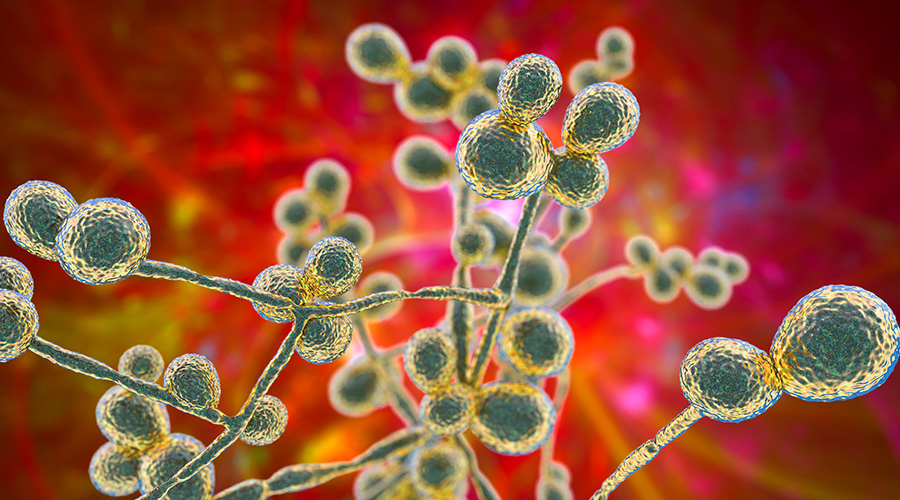 Mature Dry Surface Biofilm Presents a Problem for Candida Auris
Mature Dry Surface Biofilm Presents a Problem for Candida Auris Sutter Health's Arden Care Center Officially Opens
Sutter Health's Arden Care Center Officially Opens Insight Hospital and Medical Center Falls to Data Breach
Insight Hospital and Medical Center Falls to Data Breach The High Cost of Healthcare Violence
The High Cost of Healthcare Violence EVS Teams Can Improve Patient Experience in Emergency Departments
EVS Teams Can Improve Patient Experience in Emergency Departments