A new report has identified key risks and opportunities in current structures, processes and outcomes at New York hospitals as a result of the COVID-19 pandemic. The report from the Healthcare Association of New York State’s statewide steering committee on quality initiatives is entitled, “COVID-19 Lessons Learned in New York’s Hospitals.”
In spring 2020, New York was at the epicenter of the COVID-19 pandemic. The crisis revealed healthcare inequities, differences in capacity to respond between small and large organizations, and an inability to continue routine care. The association’s committee, composed of hospital and health system quality, clinical and patient safety experts, performed a thorough, systematic root-cause analysis. The group identified underlying system and process causes and contributing factors that resulted in an overwhelmed healthcare delivery system. The report’s key findings in two key facility-related areas:
Environment of care: “COVID-19 profoundly changed the environment of care experienced by New Yorkers. The need for quarantine and infection control reduced access to most non-COVID-19 medical services and made hospitals off limits to families and visitors. The new physical environment delivered care in tents and from behind plexiglass barriers, while “load sharing” shifted patients among facilities and geographic regions. When the pandemic interrupted in-person care delivery, telehealth initiatives grew to satisfy patient needs for care in the new healthcare environment.”
Equipment: “Ineffective supply chain management systems, including just-in-time inventory and single source suppliers, led to demand far exceeding supply for many critical tools and treatments. Along with price gouging, this increased the likelihood of inequitable dissemination of supplies for many institutions, harm, and an overwhelmed healthcare delivery system.”

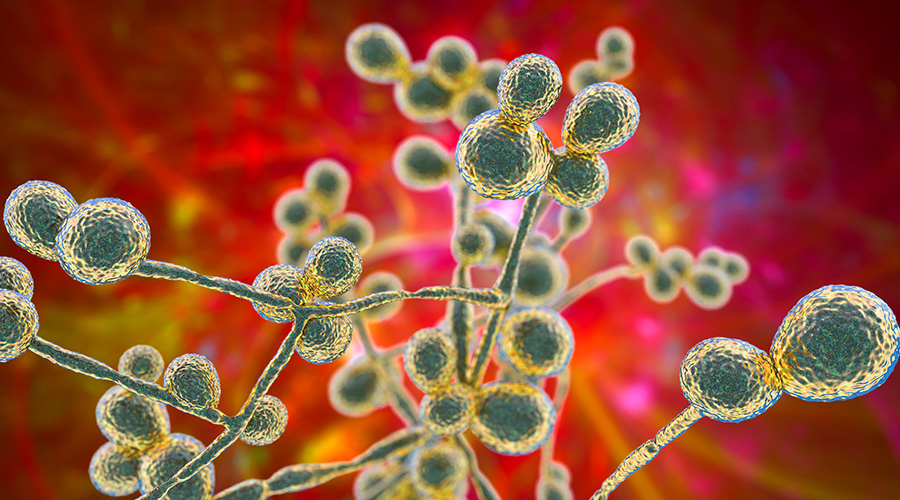 Mature Dry Surface Biofilm Presents a Problem for Candida Auris
Mature Dry Surface Biofilm Presents a Problem for Candida Auris Sutter Health's Arden Care Center Officially Opens
Sutter Health's Arden Care Center Officially Opens Insight Hospital and Medical Center Falls to Data Breach
Insight Hospital and Medical Center Falls to Data Breach The High Cost of Healthcare Violence
The High Cost of Healthcare Violence EVS Teams Can Improve Patient Experience in Emergency Departments
EVS Teams Can Improve Patient Experience in Emergency Departments