Texas hospitals are running out of intensive care unit (ICU) beds as the COVID-19 surge is becoming the largest of the entire pandemic, according to the Texas Tribune. One-half of the state's 22 trauma service areas reported 10 or fewer open beds as of Aug. 8. More than 9,400 COVID-19 patients fill the state’s ICUs. The federal government reported that at least 53 Texas hospitals have no ICU capacity during the week ending Aug. 5.
In Austin, five hospitals were at or above 90 percent of ICU capacity in the same period. Harris Health System in Houston recently reported that 25 percent of patients at its two hospitals have tested positive for COVID-19, according to CNN. State hospitals are seeing more younger people in beds, likely due to the surging delta variant. Patients in ICUs are staying in the hospital longer than expected compared to previous surges.
About 87 percent of all hospital beds in Texas are in use, according to Newsweek. 14.1 percent of those beds are occupied by COVID-19 patients. This is the highest percentage of beds taken since the beginning of the pandemic. Lyndon B. Johnson Hospital is setting up tents and installing the proper equipment to handle an influx of patients. This hospital is using all of its ICU beds, 63 percent of which are occupied by COVID-19 cases.
This latest surge comes at a time when Texas is experiencing a staffing crisis due to burnout from the ongoing pandemic. Nurses are leaving due to better paying jobs in the increasingly competitive market. There are 23,000 more unfilled registered nurse jobs in the state than there are nurses seeking to fill them, according to the Texas Workforce Commission.
One hospital system in Central Texas reported a 25 percent turnover in the past year. Most full-time Texas nurses at hospitals are paid about $75,000, which is in line with the national average. Hospitals are losing nurses who choose to become traveling contractors for higher pay or who go to larger hospitals. Competition means smaller hospitals that can’t afford to pay nurses more are suffering, making their fight against COVID-19 tougher.

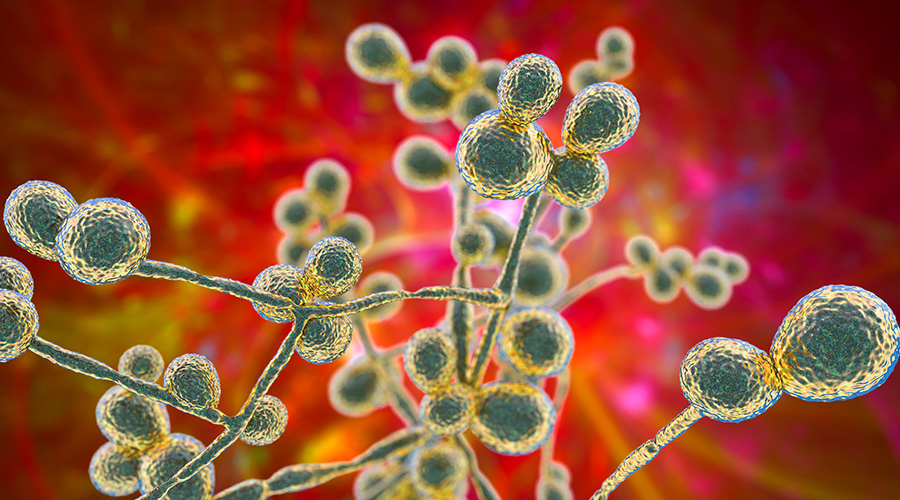 Mature Dry Surface Biofilm Presents a Problem for Candida Auris
Mature Dry Surface Biofilm Presents a Problem for Candida Auris Sutter Health's Arden Care Center Officially Opens
Sutter Health's Arden Care Center Officially Opens Insight Hospital and Medical Center Falls to Data Breach
Insight Hospital and Medical Center Falls to Data Breach The High Cost of Healthcare Violence
The High Cost of Healthcare Violence EVS Teams Can Improve Patient Experience in Emergency Departments
EVS Teams Can Improve Patient Experience in Emergency Departments