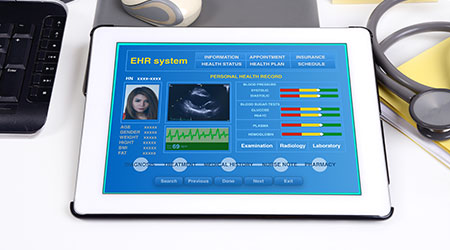
‘EHR integration’ is still a phrase that can quickly change the mood of a conversation. Most everyone has a few battle scars from a challenging integration project, but it is important to remember that not every integration requires a moonshot effort and without integrations, the impact potential of technology is limited. Many hospitals are not reaping the full benefits of their patient-facing technology because they either failed to plan for EHR integrations or they aren’t implementing them efficiently or in a scalable manner.
Why integrate with the EHR?
Value-based care makes patient experience a priority. For over 10 years, research has shown informed patients who are active in their own care measures have a better experience and better outcomes. Research also indicates that as patient activation levels change costs go up or down accordingly. Investments into patient facing-technology with the potential to influence patient experience and activation levels (e.g. education, med library, meal choices, digital whiteboards, wearables, messaging) make sense. However, technologies that are not well-integrated usually deliver a poor user experience and are less utilized than integrated systems. The investment falls short of its potential.
Well-integrated technology not only puts less burden on staff but also increases workflow efficiencies. Fewer redundant processes, like data entry, reduce human error and allow clinical staff more time for direct care (also a significant factor in value-based care). The biggest advantages of data-driven care will come from better connecting patients with those most able to care for their conditions.
Electronic health records should serve as the single “point of truth” and this requires a strategy of data flowing out and data returning to the EHR. The trustworthiness of the data depends on it being current. The EHR data must export to other systems, interact with those systems, return from those systems and update the EHR accordingly. The EHR then presents an accurate and reliable truth. The real power of the EHR lies in this ability.
EHR integrations enable both the quantity and quality data needed for continued and scaled advancements. Thanks to initiatives like Meaningful Use, nearly all hospitals have EHR technology in place, but far fewer leverage integrations. Planning early for integrations and with a vision of interoperability is key to changing patient experience. Speaking with vendors and consultants is helpful for discovering more ways your EHR can share data with other systems to create a cohesive, integrated technology platform.
Build one system, not a collection of silos
Plan for expansion phases to include key integrations such as a HL7 ADT feed for systems that leverage patient info as well as an HL7 or XML interface back into the EHR. This will allow you to leverage interface messaging for all kinds of things including orders, results, schedule/procedure information, discharge information, progress notes, and CCD. Leveraging common integration standards such as HL7, FHIR, and XML/Web API integrations, file transfers, database reads/writes keeps costs down as there is less customization required.
Another cost and efficiency strategy is to use fewer APIs by striving for platform-level integrations instead of application-level integrations. A platform level API is much like a power strip for code but instead of reducing the chaos of extension cords and adaptors, it manages the clutter and reduces the failure points of strings of code. It provides a communication exchange hub for systems to simply plug into. This also streamlines testing as you can routinely test one larger API rather than small changes every time a vendor makes an update. You are creating a single environment where the technology coexists.
Rely on vendors (but don’t overpay)
Many facilities waste a lot of time and money trying to start from scratch and building their own interfaces to work with someone else’s solution.
Interactive Patient System (IPS) vendors have integration experience. Along with knowing the capabilities of their own systems, they also know EHRs and 3rd party systems and can quickly identify integration possibilities. Remember, your system is the single point-of-truth and vendors should adapt to integrate with your existing integration ecosystem.
Set expectations early that integrations are required and ask vendors to build them where possible. Instead of spending your resources building integrations, leverage your experience with testing, training and rolling out updates to ensure successful integrations. If you learn what 3rd party integrators charge for similar integration builds, you can make sure your vendor has reasonable fees.
Healthcare facilities can dramatically change patient experience by embracing a strategy of ever-increasing interoperability particularly as related to EHR integrations. Having an integration plan allows a facility to budget time and resources accordingly. It guarantees your system will continually contribute to a positive patient experience.
Brad Storm is the vice president of healthcare technology & integrations for SONIFI Health.
 Biofilm 'Life Raft' Changes C. Auris Risk
Biofilm 'Life Raft' Changes C. Auris Risk How Healthcare Restrooms Are Rethinking Water Efficiency
How Healthcare Restrooms Are Rethinking Water Efficiency Northwell Health Finds Energy Savings in Steam Systems
Northwell Health Finds Energy Savings in Steam Systems The Difference Between Cleaning, Sanitizing and Disinfecting
The Difference Between Cleaning, Sanitizing and Disinfecting Jupiter Medical Center Falls Victim to Third-Party Data Breach
Jupiter Medical Center Falls Victim to Third-Party Data Breach