The ongoing labor shortage is impacting every single industry, and the hospitals and other healthcare facilities are not exempt from it. Healthcare employees are quitting in record numbers citing burnout, lack of flexibility and poor treatment as reasons to leave. However, hospitals are now struggling to recruit and retain new talent, resulting in some locations or wards being at risk of shutting down because of lack of staff.
As Healthcare Facilities Today previously reported, Advocate Aurora Health temporarily closed three urgent care facilities in the Milwaukee area in December due to staffing issues. Also, Indiana’s Pulaski Memorial Hospital closed its OB department in March – an action brought on by the impact of the COVID-19 pandemic and lack of available maternity nurses.
Meanwhile, long-term care facilities are also hurting from the labor shortage. Since the beginning of the pandemic, employment levels in nursing homes have dropped by 14 percent. In comparison, hospitals have lost just 1.6 percent of employees. According to the report by American Health Care Association and National Center for Assisted Living, 86 percent of nursing homes and 77 percent of assisted living providers have said that their workforce situation has gotten worse in recent months, forcing 58 percent of nursing homes to begin limiting new admissions. In addition, 78 percent of nursing homes and 61 percent of assisted living communities are concerned workforce challenges might force them to close their operations.
These aren’t the only healthcare facilities at risk of closing. There are over 500 rural hospitals at immediate risk of closure due to financial losses and lack of financial reserves to sustain operations, according to a report by the Center for Healthcare Quality and Price Reform. . Almost every state has at least one rural hospital at immediate risk of closure, and in 21 states, 25 percent or more of the rural hospitals are at risk.
Nearly all the rural hospitals that are at risk of closing are in isolated rural communities. If closed, community residents would no longer be able to receive emergency or inpatient care without having to travel long distances. Meanwhile, these facilities are often the only place residents can get laboratory tests or imaging studies done.
The American Hospital Association is urging Congress to address the ongoing staffing shortage in a statement submitted to the Senate Health, Education, Labor & Pensions Committee. In it, the agency discussed the way it is impacting hospitals and health systems, detailing ways the field is supporting its workforce and asking Congress to enact policies to address the issue.
“Though managing workforce pressures were a challenge for hospitals even before the pandemic, these challenges have only grown more acute,” the statement says. “The incredible physical and emotional toll that hospital workers have endured in caring for patients during the pandemic has, among other issues, exacerbated the shortage of hospital workers. This shortage has become so critical that some states and the federal government have deployed military and National Guard resources to help mitigate staffing challenges at some hospitals. As this shortage has worsened and COVID-19 hospitalizations have reached record levels, labor costs for hospitals have increased dramatically. This combination of factors has been exploited by traveling staffing companies and other firms that provide contract labor resources, driving up workforce slots even more for hospitals. Hospitals also have incurred significant costs in recruiting and retaining staff, which have included overtime pay, bonus pay and other incentives. This is occurring at a time when many hospitals and health systems are still facing other immense financial constraints. For many hospitals around the country, this has led to an unsustainable situation that threatens their ability to care for the patients and communities they serve.”
Mackenna Moralez is assistant editor with Healthcare Facilities Today.

 Reframing the Construction Manager as a Community Manager
Reframing the Construction Manager as a Community Manager Health First Celebrates 'Topping Off' Ceremony for New Cape Canaveral Hospital Campus
Health First Celebrates 'Topping Off' Ceremony for New Cape Canaveral Hospital Campus The University of Hawai'i Cancer Center Caught Up in Cyberattack
The University of Hawai'i Cancer Center Caught Up in Cyberattack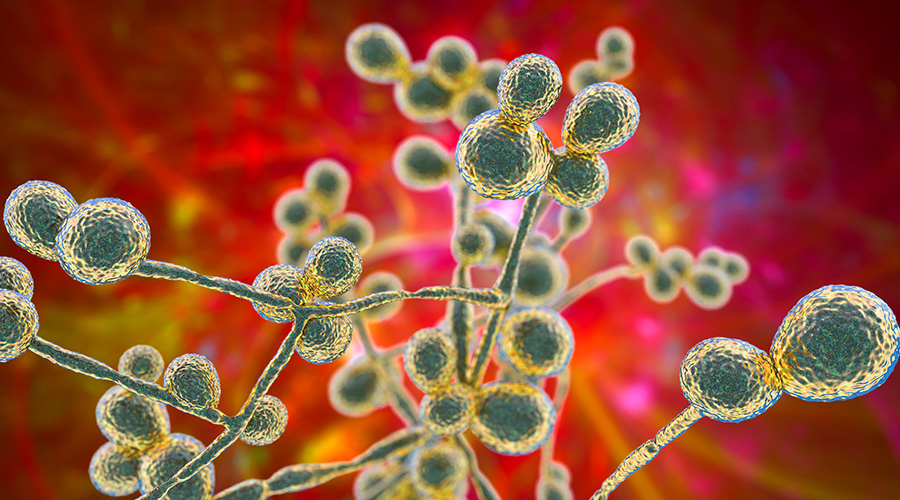 Mature Dry Surface Biofilm Presents a Problem for Candida Auris
Mature Dry Surface Biofilm Presents a Problem for Candida Auris Sutter Health's Arden Care Center Officially Opens
Sutter Health's Arden Care Center Officially Opens