Even though telehealth has been around for decades, the pace of adoption has historically varied among provider organizations. That is, until COVID-19 changed everything, and out of necessity, providers began delivering virtual care on a much greater scale.
Telehealth has become an integral part of healthcare delivery, even as the pandemic subsides. Patients and clinicians have embraced the convenience, flexibility, and safety of receiving and providing care anywhere – from homes and outpatient clinics to hospitals and other venues.
The Centers for Medicare and Medicaid Services (CMS) and other payers greatly expanded reimbursement for telehealth visits during the pandemic. Many of these temporary changes are likely to become permanent, supporting continued telehealth growth.
Virtual care models have a major impact on facility design and planning, but historically there has been minimal guidance on how to effectively integrate them into facilities. As always, the primary goal should be to create resilient facilities that promote optimal functionality, productivity and profitability while easily adapting to healthcare’s constantly evolving technology, care models and trends.
The key inputs that typically drive facility and capacity planning include projected patient volumes, provider and service complements, and operational and care models. But these issues alone are not sufficient to account for increased telehealth utilization when planning a new outpatient facility. Several other factors should be integrated within the planning process.
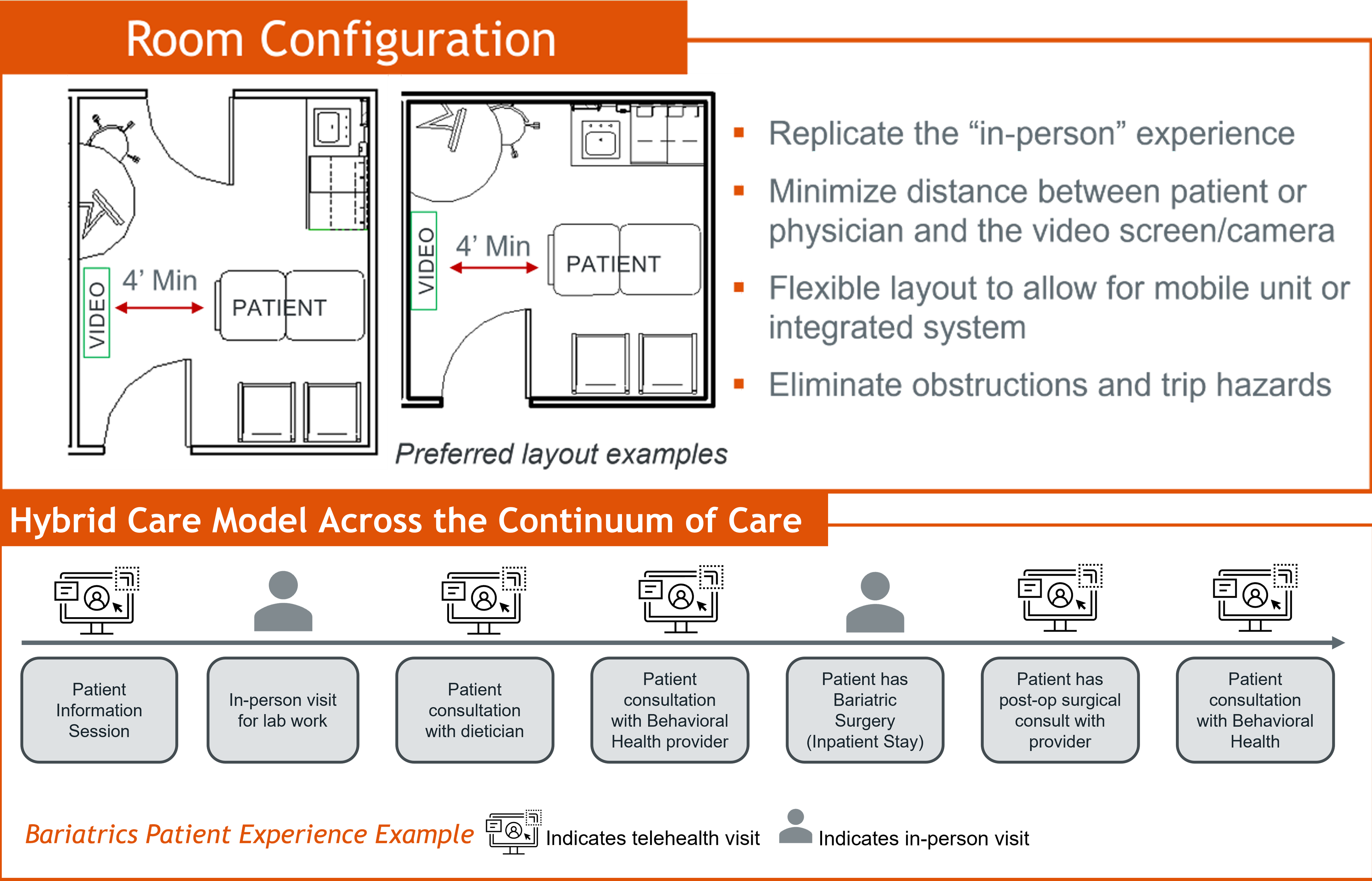
Hybrid care. A hybrid care model is the emerging standard of care. Delivering a mix of in-person and virtual care is becoming the standard of care for most specialties. As technology evolves, providers can deliver cognitive and procedure-based services through telehealth.
Digital peripherals that monitor biometric data, such as weight scales, pulse oximeters, digital stethoscopes, exam cameras, and blood pressure cuffs make this possible. Patients can self-administer their diagnostics at home while a remote provider interprets the data to determine if treatment or medication adjustments are needed. This approach enables the care team to better coordinate and deliver care to patients across the continuum.
Let’s look at a bariatrics patient for example. The patient journey might begin with an information session, either in-person or conducted virtually, followed by an in-person visit for lab work. The patient then can have either telehealth or in-person consultations with a dietician and a behavioral health provider to prepare for surgery. While the procedure is performed in a hospital or ambulatory surgery facility, much of the post-op care can be delivered in a patient-preferred setting. The combination of in-person and virtual care demonstrates the flexible hybrid care model fully integrated into an outpatient practice environment.
Outpatient considerations. A telemedicine session doesn’t necessarily replace an in-person outpatient visit. There isn’t necessarily a one-to-one replacement of telemedicine visits with in-person visits. This is key when determining capacity for a new outpatient facility and recognizing that increased telehealth utilization may not reduce the need for physical space.
Take the example of a patient who has either a chronic condition, such as congestive heart failure, or was discharged from a hospital where vitals might be measured from home with digital peripherals. When remote providers interpret the data, they might determine that an outpatient visit is needed. While this might avoid a costly hospital trip or readmission, it could drive an additional outpatient visit. Merely assuming that telehealth utilization of 30 percent requires 30 percent less space might result in an undersized facility.
Success in the details. For ambulatory care facilities, delivering a high-quality, satisfying telehealth experience for the patient and the clinician means paying attention to numerous design details. These include:
- Exam room configuration. Optimizing the video experience requires locating the camera directly across from the exam table, minimizing the distance between the patient or physician, the camera and video screen, and allowing enough space for clinicians to move around the patient without obstructing the view.
- Lighting. Direct and indirect warm white light creates a clear, shadow-free image of the patient. Avoid harsh LED, fluorescent and natural lighting that can wash out complexions. When developing a new facility, consider a windowless interior location to maximize lighting control.
- Acoustics. To protect privacy, build rooms to contain noise, since people tend to speak more loudly on video. Upgrade wall and ceiling construction to STC 50-55, and install door gaskets, a sound-masking system, and sound-absorbing panels.
- Background. Keep it clean, professional, and uncluttered. Light blue or gray tones are ideal, and use flat paint to eliminate glare.
- Power. Install multiple four-plex outlets to allow for flexible location of equipment and avoid creating trip hazards. A back-up power source is also critical for uninterrupted connectivity.
Technology matters. To closely replicate the in-person experience, facilities need the right equipment and IT infrastructure. Large, high-definition monitors and cameras are must-haves, as are noise-canceling microphones and headsets. Physicians should have dual monitors – one for seeing the patient on screen and the other for viewing medical records and data. Although a wired connection works best, wireless access points also should be installed in exam rooms and hallways to support Wi-Fi. Install data outlets next to all electrical outlets and consider a secondary internet service in case of an outage.
Measurable investment. Designing ambulatory facilities versatile enough to support a hybrid model generates an excellent return on investment and value of investment from the estimated additional up-front costs – $5,000-7,500 per exam room – when planning a new facility, especially when considering direct revenue and downstream cost savings.
For example, providers might be able to increase the total number of patients seen, and better management of patient conditions can reduce avoidable emergency department visits and readmissions. As telehealth becomes embedded across the care continuum, it makes smart business sense to integrate it into facility planning and invest upfront in flexible solutions that build sustainable success.
Eric Carmichael is principal and Chris Lambrecht is senior vice president of construction and development with MedCraft Healthcare Real Estate. Bryan Arkwright is co-founder and chief research officer with Cromford Health.

 What 'Light' Daily Cleaning of Patient Rooms Misses
What 'Light' Daily Cleaning of Patient Rooms Misses Sprinkler Compliance: Navigating Code Mandates, Renovation Triggers and Patient Safety
Sprinkler Compliance: Navigating Code Mandates, Renovation Triggers and Patient Safety MUSC Board of Trustees Approves $1.1B South Carolina Cancer Hospital
MUSC Board of Trustees Approves $1.1B South Carolina Cancer Hospital Study Outlines Hand Hygiene Guidelines for EVS Staff
Study Outlines Hand Hygiene Guidelines for EVS Staff McCarthy Completes $65M Sharp Rees-Stealy Kearny Mesa MOB Modernization
McCarthy Completes $65M Sharp Rees-Stealy Kearny Mesa MOB Modernization