When the following alert popped up on my phone, it had my immediate attention: “Deadly Fungus in U.S. Hospitals Isn’t Fiction.” This drug-resistant yeast, Candidozyma auris (C. auris), is invading patient rooms, hiding on surfaces and surviving cleaning procedures that once protected patients. For patients who are already weak, it might be too much.
The hospital is supposed to be a place to heal. Now it is becoming a dangerous place to be for some patients. Those with central lines, urinary catheters, ventilators, feeding tubes and extended hospital stays face the greatest risk.
A new survey from the European Center for Disease Prevention and Control (ECDC) warns of a sharp rise in C. auris cases across Europe. European Union and European Economic Area countries recorded about 4,012 cases between 2013 and 2023, with more than one-half of them reported just in the past two years. The ECDC warns that once endemic transmission is established, the window of effective intervention narrows rapidly.
The problem is not confined to Europe. A total of 10,788 clinical cases were recorded in the United States between 2016 and 2023, the most recent year for which the U.S. Centers for Disease Control and Prevention (CDC) has collected data on C. auris. New York, Illinois, California, Florida and Nevada reported the highest number of cases — more than 1,000 each.
These cases are clinical ones, referring to “patients with C. auris identified in a sample tested to find out the cause of an infection.”
Another 22,931 screening cases were reported, referring to patients who received a positive C. auris result from a swab collected to test for colonization. Colonization refers to C. auris on the skin and other body sites without symptoms. But “people who are colonized can spread C. auris onto to surfaces and objects around them and to other patients,” according to the CDC.
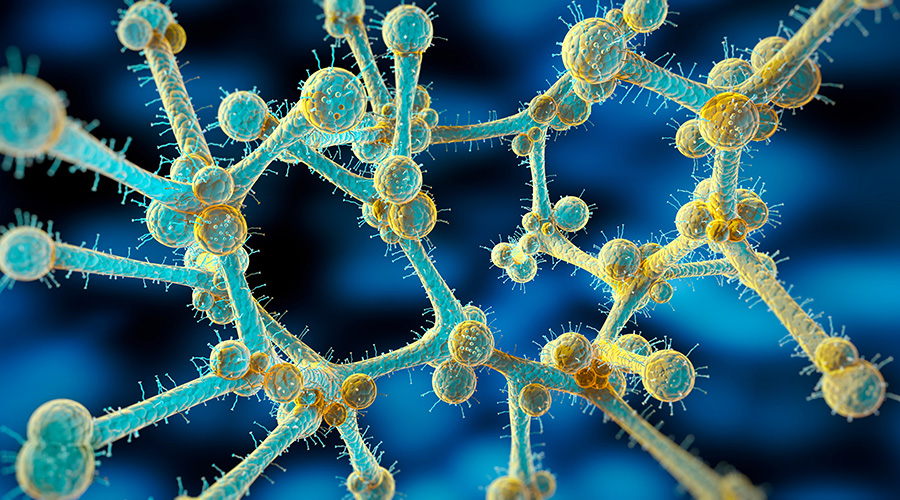
C. auris is particularly difficult to control because it produces its own biofilm on hospital surfaces. These biofilms make C. auris and other so-called superbugs more dangerous. Microbes adhere to patient equipment, supplies and environmental surfaces and create protective biofilms as a barrier against the external environment, including most disinfectants.
Also, different pathogens often colonize the same biofilm and exchange antibiotic-resistant genes, making infections even more difficult to treat. Organisms living in biofilms can survive on surfaces for two-four weeks and be up to 1,500 times less susceptible to disinfectants.
The list of microbes — including gram-positive and gram-negative bacteria and fungi — that can cling to surfaces and medical devices in biofilms is long and diverse. In fact, the superbugs that contribute to most healthcare-associated infections (HAI) can persist in armor-like biofilms created by C. auris.
The list of surfaces where biofilms persist is also long and diverse. In addition to countertops and other hard surfaces, the list includes floors, stainless steel, plastic, textiles, and portable medical equipment shared between patients. Here are a few suggestions for controlling C. auris in a facility:
- Focus on cleaning and disinfecting high-risk surfaces most prone to biofilm formation, including reusable and shared equipment.
- Consider cleaning a C. auris isolated patient’s room twice daily.
- Search the disinfectants on the EPA List P: Disinfectants Effective Against C. Auris.
- Before selecting a disinfectant from that list, read the master label to ensure that the product kills bacteria in biofilm. The biocidal agent should have a contact time of less than three minutes and be EPA registered as effective against biofilm while having efficacy claims against a broad spectrum of pathogens, including C auris.
J. Darrel Hicks, BA, MESRE, CHESP, Certificate of Mastery in Infection Prevention, is the past president of the Healthcare Surfaces Institute. Hicks is nationally recognized as a subject matter expert in infection prevention and control as it relates to cleaning. He is the owner and principal of Safe, Clean and Disinfected. His enterprise specializes in B2B consulting, webinar presentations, seminars and facility consulting services related to cleaning and disinfection. He can be reached at darrel@darrelhicks.com, or learn more at www.darrelhicks.com.
 Regulations Take the Lead in Healthcare Restroom Design
Regulations Take the Lead in Healthcare Restroom Design AHN Allegheny Valley Hospital Opens Expanded Inpatient Rehabilitation Unit
AHN Allegheny Valley Hospital Opens Expanded Inpatient Rehabilitation Unit HSHS and Lifepoint Rehabilitation Partner on New Inpatient Rehab Hospital in Green Bay
HSHS and Lifepoint Rehabilitation Partner on New Inpatient Rehab Hospital in Green Bay Turning Facility Data Into ROI: Where Healthcare Leaders Should Start
Turning Facility Data Into ROI: Where Healthcare Leaders Should Start Sutter Health Breaks Ground on Advanced Cancer Center and Care Complex
Sutter Health Breaks Ground on Advanced Cancer Center and Care Complex