A new ATI Advisory analysis commissioned by the National Investment Center for Seniors Housing & Care highlights a history of often uncoordinated policy decisions that have resulted in a failure to attract needed capital to modernize skilled nursing facilities. The results — often outdated buildings and low innovation — are substantial barriers to adequately caring for and housing frail, older adults, experts say.
They say federal policymakers should address the root cause of facilities’ inefficiencies: misalignment of the public-private partnerships that attract capital to own skilled nursing facility real estate instead of investing in innovating operations and modernizing facilities.
The analysis finds that public-private partnerships, created to help Americans access their Medicare and Medicaid benefits and which supported skilled nursing facilities for 50 years, are failing. Medicaid reimbursement rates in many states are insufficient to cover the cost of care, causing facilities to leverage higher reimbursement from Medicare patients to subsidize shortfalls. Increasingly, beneficiaries are replacing Medicare with Medicare Advantage, which reimburses 20 percent less on average than traditional Medicare.
Challenges resulting from less reimbursement from federal programs means ready access to private capital is crucial to remedying skilled nursing facilities’ challenges, the experts say.
The analysis says federal policymakers should consider four key strategies to improve skilled nursing facilities:
- Adopt measures to improve labor supply and retain the existing labor pool. Staffing levels pose the biggest challenge to operators and policymakers, so support for educational institutions and prospective students could promote a steady flow of individuals into long-term care professions.
- Incentivize innovation. A more coordinated, predictable reimbursement model combined with U.S. Department of Housing and Urban Development financing policies that incentivize modernization and innovation could attract long-term capital to support long-term innovation and investments.
- Embrace new quality measures to improve transparency. Quality measures should reward superior operators, promote transparency, support more predictability in a heavily regulated market and incentivize private capital to enter the industry.
- Support access to capital. America’s aging population is rapidly increasing. The government alone cannot meet the capital needs of skilled nursing facilities. Private funding plays a crucial role in enabling access to Medicare and Medicaid benefits designed to serve the frail elderly in skilled nursing facilities.

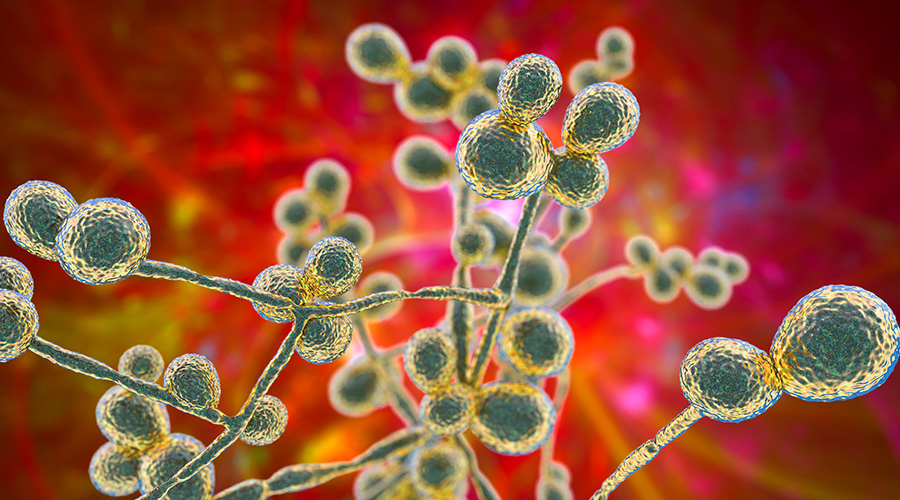 Mature Dry Surface Biofilm Presents a Problem for Candida Auris
Mature Dry Surface Biofilm Presents a Problem for Candida Auris Sutter Health's Arden Care Center Officially Opens
Sutter Health's Arden Care Center Officially Opens Insight Hospital and Medical Center Falls to Data Breach
Insight Hospital and Medical Center Falls to Data Breach The High Cost of Healthcare Violence
The High Cost of Healthcare Violence EVS Teams Can Improve Patient Experience in Emergency Departments
EVS Teams Can Improve Patient Experience in Emergency Departments